Other Issues
Other medical issues your baby may experience
There are many medical issues your baby may experience. Here, we will cover:
- Cleft lip and palate
- Neonatal Abstinence Syndrome
- Jaundice
- Retinopathy of Prematurity
- MRSA
- Low Blood Sugar
- Vomiting
- Down Syndrome
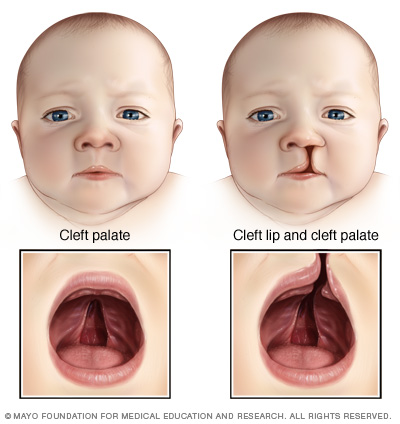
Cleft Lip and Palate
A cleft lip is an opening in the lip while a cleft palate is an opening in the roof of the mouth. A cleft lip or palate forms due to the incomplete development of the lip or palate while the baby is forming before birth. During the first three months of pregnancy, the lip develops in two parts; the right-hand side and then the left-hand side. The two parts continue to develop towards each other until they meet and join/fuse together.
This can be seen as the vertical line in the centre of the upper lip or the line running from front-to-back at the centre of the roof of the mouth. Sometimes, this fusion gets interrupted: it is not known why this happens, and it is not because of anything you did during pregnancy. It may be a result of a genetic predisposition and some cleft lips/palates occur in combination with other medical issues or syndromes. Often cleft palates are diagnosed during pregnancy with an ultrasound.
If your baby has been born with a cleft lip or palate, you may have feelings of concern, distress, anxiety, and/or worry about it. Do talk about your feelings and concerns with your baby’s nurse and doctor. A team of specialists will provide you and your baby with the care you require and will develop a plan or care/treatment.
Your baby’s cleft lip/palate is best managed by a team of medical, surgical, dental, speech, and other specialists. Depending on the severity of the condition, surgery may be required. Surgical repair will be carried out within a few months of birth. It will either occur in stages as your baby grows and develops or as a once off elective procedure.
Feeding Your Baby with A Cleft Palate
Depending on the severity of the condition, you may face challenges when feeding your baby. If you are planning to breastfeed, it is important to establish feeding as soon as possible and to monitor your baby’s weight gain. This is especially important if surgical repair of the cleft palate is planned. Should you plan to feed your baby by bottle, special teats/nipples and squeeze bottles may be required. The speech and language therapists will help you to establish feeding. They will also follow-up with your baby as they grow and will provide speech therapy.
Babies with cleft palates tend to tire easily turning feeds and feeding may take longer than you would expect. Your baby may feed noisily and often swallow a lot of air. This can lead to colic and wind. During and after feeds, they may spit milk that has come down from the nose. Your baby may also be prone to ear infections. Offering your baby small, frequent feeds may help with these challenges. If your baby is experiencing difficulties with oral feeding, a nasogastric/orogastric tube may be inserted to ensure adequate hydration.
More information can be found on www.cleft.ie and www.irishhealth.com/psg/cleft
Neonatal Abstinence Syndrome
Neonatal abstinence syndrome (NAS) is a group of symptoms a baby may experience as a result of exposure to drugs in pregnancy, such as narcotics, opiates, medicinal products, or prescription products, and/or as a result of high volumes of products ingested, such as caffeine. Exposure during pregnancy may lead to the baby developing withdrawal symptoms for a period of time when the umbilical cord is cut, which stops the supply.
Symptoms of NAS/withdrawal include: restlessness, tremors/jitters/shakes, poor sleeping, excessive sucking, low-grade temperature, sweaty, vomiting, diarrhoea, poor weight gain, poor feeding, yawning and snuffles, a high pitched and often excessive crying, tight muscle tone, rapid breathing, and, in severe cases, seizure activity. These symptoms of withdrawal are rarely obvious initially but become evident after a few days after birth.
The aim when treating a baby with NAS is to reduce irritability and improve feeding. Your baby’s nurse will score the severity of the symptoms using a scoring chart called the ‘Finnegan Score’. Based on this score, your baby’s treatment will be decided upon by the doctor (consultant neonatologist) on duty. Generally, Oromorph (an oral morphine solution), Clonazepam, and Phenobarbitone are the treatments used. The doses prescribed for these treatments will vary depending on the weight of the baby and on the severity of symptoms exhibited by them. Once the symptoms have been controlled, the treatment dose is gradually reduced every 3 to 4 days.
If your baby is experiencing withdrawal, they will be swaddled in a single sheet or blanket and nursed in a quiet, dimly lit area. Barrier creams will be applied to their buttocks to reduce risk of excoriation from potential continuous diarrhoea. They will receive a high energy formula feed in frequent, small amounts to ensure adequate weight gain.
The decision as to when your baby can go home is made by the named consultant neonatologist, based on your baby’s medical and social circumstances. Discharge plans may involve support services and pharmacy arrangements if required.
Jaundice
Jaundice is also known as ‘hyperbilirubinemia’. It is one of the most common conditions requiring medical attention in both term and preterm babies. It refers to the yellow colouration of the skin as well as the whites of the eyes. In general, yellowing of the skin starts in the face and works its way down to the feet. Jaundice is caused by the accumulation of bilirubin in the skin and mucous membranes. It is mainly due to the immaturity of the liver and immature fragile red blood cells. For most babies, jaundice is not an indication of an underlying disease and is generally harmless. Usually, it resolves as the baby matures and develops.
Preterm babies have a greater chance of developing jaundice than term babies. Approximately 60% of term and 80% of preterm babies develop jaundice within the first week of life [1]. Breastfed babies are more likely than bottle-fed babies to develop physiological jaundice within the first week which may persist beyond the first 14 days. Approximately, 10% of breastfed babies remain jaundiced at 1 month. In general, prolonged jaundice is harmless, however, in some cases, it can be an indication of serious liver disease.
There are many other possible causes of jaundice including blood group incompatibility between your blood and your baby’s blood, most commonly Rhesus or ABO group incompatibility; haemolysis, i.e. the breaking down of red blood cells; sepsis, i.e. infection; liver disease; bruising; and metabolic disorders. One other cause is the lack of a particular enzyme which can cause severe neonatal jaundice. However, this generally runs in families and is more prevalent in certain ethnic groups.
What is bilirubin?
Bilirubin a yellow compound/pigment produced from the breakdown of red blood cells. It’s mostly ‘bound’ to a protein in the blood and the majority of it is excreted in the baby’s stools. However, some of it is ‘free’, or not bound, and has the potential to pass through a membrane that separates the blood from the brain, the blood-brain barrier. This can be toxic to the brain and spinal cord which can lead to both short- and long-term neurological issues. The risk of this happening is increased in babies with extremely high bilirubin levels which is referred to as Kernicterus.
Recognising jaundice can be difficult, particularly in babies who have darker skin tones. However, the palms of the hands and soles of the feet along with the colour of the urine and stools provide further indication of jaundice. The level of bilirubin in a baby’s blood can be measured using a small device called a bilirubinometer. This hand held device beams light onto the baby’s skin and calculates the amount of bilirubin in the blood based on how much light is absorbed and reflected by the skin. Alternatively, blood tests are taken to measure the level of bilirubin. The blood test also determines if certain antibodies or proteins are present on the surface of the red blood cell. This test is called Direct Coombs Test, or DCT. Once the presence and severity of jaundice have been recognised, the baby is treated by placing them under phototherapy.
Phototherapy, or ‘light therapy’, involves exposing the jaundiced baby to a special light source unit. During phototherapy, the baby is not clothed and will have their eyes covered with eyes pads to protect them from the bright light. The light may be white, blue, or green. A single light source or multiple sources of light may be used depending on the level of bilirubin in the blood and the gestational age of the baby. Phototherapy is usually needed for a few days and is continued until the level of bilirubin drops below a treatment line and remains at this lower level for a minimum of six hours.
The lights may cause a mild rash, but this quickly heals when phototherapy stops. Treatment will break down the bilirubin which will be excreted in the baby’s stool (poo). As the baby matures, the ability of their liver to break down bilirubin will increase. Finally, if you arrive at the neonatal unit (NNU) when your baby is receiving phototherapy, the nurse will temporarily stop therapy. As you are an essential part of your baby’s development, your time time together is better spent for skin-to-skin contact, cuddles, and feeding.
Retinopathy of Prematurity
Retinopathy of prematurity, or ROP, is frequently seen in premature babies. It’s caused by the development of abnormal blood vessels in the eye which can if left untreated, lead to loss of vision. Not all premature babies will have ROP screening as it is dependent on gestational age, birthweight, and is at the discretion of the consultant. If your baby weighs less than 1,500g, or was born before 32 weeks’ gestation, they are at risk of ROP and will be screened.
An eye specialist doctor (an ophthalmologist) will check your baby for ROP. To carry out the screening, eye drops are prescribed and instilled into your baby’s eyes which cause the pupils to dilate. Then, your baby will be examined by a specialist doctor within a few hours. Prior to examination, the doctor will check your baby’s identification bands and insert ‘numbing drops’ into your baby’s eyes. Your baby will be given a small amount of sucrose called ‘Sweeteze’ into their mouth to ease the discomfort. A small instrument may be used to help keep the eye open for examination. It is not painful for your baby but may be uncomfortable.
The result of the examination will be discussed with you as well as any plans for further monitoring. This screening ensures early detection of abnormal vessels so early treatment is possible which increases the likelihood of a positive outcome for your baby.
If ROP is present, the ophthalmologist will treat the condition with laser treatment. If this treatment is not available in the hospital, your baby may need to be transferred to another hospital. In some instances, the ophthalmologist may choose to freeze the retina with cryotherapy, rather than using a laser. For cryotherapy, your baby will be sedated or given a general anaesthetic for the procedure.
In general, the outcome from ROP treatment is very successful. However, some cases do result is minor vision impairment such as short-sightedness that will require glasses, ‘crossed eyes’ (strabismus) or a ‘lazy eye’ (amblyopia) which will need the use of an eye-patch to correct the condition.
MRSA
Staphylococcus aureus is a bacterium that approximately 30% of people carry on their skin or in their noses. It is spread by direct skin-to-skin contact. Most types of Staphylococcus aureus do not cause any problems but if it does cause an infection, it can be easily treated with antibiotics such as methicillin.
Methicillin-Resistant Staphylococcus aureus (MRSA) is a strain of Staphylococcus aureus which has become resistant to methicillin which is the standard treatment of the infection. It is no more infectious than other types of bacteria, but problems arise if it enters the body through broken skin, such as operation wounds or treatment (needle) breaks in the skin. This highlights the necessity for good hand hygiene by everyone when in the hospital. Should MRSA gain access to deep tissues through broken skin, it may result in a wound infection, bloodstream infection, or ventilator-associated pneumonia if it reaches the lungs, and it can be difficult to treat.
The neonatal unit (NNU) in Cork University Maternity Hospital (CUMH) have MRSA control measures which are part of the institution-wide strategy of MRSA infection control. This is achieved in the NNU through:
- Hand hygiene: There is a policy in the NNU to educate parents and visitors to the NNU about hand hygiene. There are also adequate hand washing facilities throughout the NNU.
- Cleaning: Ensuring that the physical environment of the NNU, as well as throughout the entire hospital, is kept clean.
- NNU capacity: Taking appropriate steps to prevent patient overcrowding in the NNU as well as ensuring that there is adequate space between adjacent cots.
- Isolation rooms: There are two isolation rooms in the NNU. These are used for all transfers into the NNU from outside the hospital as well as to facilitate babies of parents that have tested positive for MRSA. Babies remain isolated until the staff in the NNU are sure that the babies MRSA tests are negative.
- Routine screening: All babies in the NNU are tested for MRSA on a weekly basis.
- Antibiotic use: CUMH follows the guidelines of the SARI Hospital Antibiotic Stewardship Subcommittee Policy which limits the use of broad-spectrum antibiotics.
- Care after discharge: To minimise the spread of MRSA, the hospital will communicate with carers, family members, general practitioners (GPs), community nurses, and community units that a patient that tested positive for MRSA and has been discharged from the hospital.
For more information about MRSA, please refer to the following link http://www.hse.ie/eng/health/az/M/Methicillin-resistant-staphylococcus-aureus/
If a baby gets infected with MRSA, they will likely be nursed for in isolation and will be treated with an antibiotic. This treatment will be given intravenously. Vancomycin is the antibiotic commonly used for the treatment of MRSA.
Low Blood Sugar
At birth, the level of sugar in the blood of a baby is similar to that of an adult. However, within a short period of time without a source of sugar, the baby’s blood sugar level drops quickly. In a healthy term baby, exclusive breastfeeding generally meets their needs which should be started within an hour after birth. This brings their sugar levels back to a normal range. If the baby cannot maintain their blood sugar levels within the normal range, the baby is said to have hypoglycaemia, or a low blood sugar level. In addition, preterm babies and very large term babies are more prone to low blood sugar levels than the term baby.
If your baby is suspected of having hypoglycaemia, they will be tested to confirm. This either involves taking blood from the heel (heel prick) or intravenously (veins). Often, hypoglycaemia results from poor feeding. If this is the reason, your baby’s feeding regime may be changed. If your baby remains hypoglycaemic after 24 hours, further investigations may be required. Babies at risk of hypoglycaemia include: small for gestational age babies; babies born prematurely; babies who are poor feeders; babies who have suffered intrapartum asphyxia, or oxygen deprivation; sick babies; large babies; and babies of diabetic mothers.
Persistent hypoglycaemia (lasting longer than 24 hours) is a cause for concern and further tests will be needed. Sometimes, the baby’s doctor will look for input from the endocrinology team. In general, the treatment for hypoglycaemia is frequent feeding but in the cases where the blood glucose remains low, or critically low, dextrose (a form of sugar) will be given intravenously. If your baby is showing signs of severe hypoglycaemia, e.g., jitteriness, being unwell, apnoea, they will immediately receive dextrose intravenously. Your baby will be gradually weaned off dextrose as they show that they can maintain their sugar level within the normal range.
Vomiting
If your baby has bile-stained vomit, it is treated as serious and possibly as a medical emergency. Your baby’s feeds will be withheld and your baby will be placed on an intravenous drip for fluids and nutrients. Your baby will be closely observed by the medical team and they may be sent for X-ray. In addition, they may be given a barium ‘meal’ during the X-ray which allows the radiologist to determine if there are any obstructions in your baby’s upper gut: their food pipe, stomach, or small intestines. Your baby will not be discharged home until the vomiting has settled down and their records reviewed by a consultant neonatologist.
In the first few days after birth, it is not unusual for blood or mucous to be present in a baby’s vomit. If this appears immediately after birth, it may be maternal blood which they have swallowed during birth and can be distinguished from fetal blood. The blood in the vomit usually looks dark red or brown and has a ‘coffee grounds’ appearance. This will not harm your baby, and will slowly work its way through your baby’s system. Blood may also be seen in your baby’s vomit if you are breastfeeding and have cracked and/or bleeding nipples.
This can occur even if there is are no obvious cracks or splits in the skin but you may have soreness when your baby is latched on. The blood in your baby’s vomit may be a pink-to-dark-red stain or look like streaks of dark brown in the vomit. The blood will not harm your baby, but you may need to get support with regard to your baby’s latch during breastfeeding, to prevent further nipple damage. Do not stop your baby from breastfeeding because of blood in breast milk. Blood in a baby’s vomit can also be caused from stress ulceration. This is common in asphyxiated babies (those that experienced oxygen deprivation).
Irrespective of the cause of vomiting, it must be remembered that vomiting can cause your baby to dehydrate very quickly and can be detrimental to their health. Whether in the hospital or at home, if you think your baby is vomiting excessively or seems well or distressed, you should seek medical advice. Vomiting in conjunction with any of the following symptoms is a cause for concern:
- Less than six wet nappies in 24 hours
- Reduced interest in feeding
- Lethargic/sluggish/exhausted behaviour
- Diarrhoea
- Fever
- The vomit has an offensive smell.
- The vomit consists of a clear, bright yellow, orange, or greenish bile fluid.
If you have concerns or questions, please talk to your baby’s nurse or doctor.
Finally, vomiting should not be confused with posseting which occurs after feeding and is the bringing back-up of milk. Milk that comes back up soon after a feed which looks, and smells, fairly similar to how it went down (a milky liquid) is simply posseting. Note: partially digested breast milk doesn’t tend to have a strong odour, but formula milk usually does.
Down Syndrome
Down Syndrome is one of the most common genetic disorders. In most cases, Down Syndrome results from altered cell division within the egg or sperm before conception. Babies born with Down Syndrome have an extra chromosome number 21, or part of that chromosome, in some or all of their cells. The cause for this altered cell division is not known. While there is an increased risk that a baby will be born with Down Syndrome in older mothers, most babies with Down Syndrome are born to mothers over 35 years of age.
Below are the most common features that a baby with Down Syndrome may show:
- Low muscle tone with an increased ability to extend their joints or a ‘floppy’ appearance
- Flat facial features with a small nose.
- Upward slant to the eyes
- Small skin folds on the inner corner of the eyes.
- Small, abnormally shaped ears.
- Single deep crease across the centre of the palm.
- Fifth finger has only one flexion furrow instead of two (on the palm side, there is only one fold on the baby finger).
- Extra space between the big toe and the second toe.
- Enlarged tongue that tends to stick out
Some babies exhibit only a few features of Down Syndrome while others exhibit many. As some of these features are also seen in babies without Down Syndrome, genetic testing must be carried out to confirm the diagnosis.
Having a baby diagnosed with Down Syndrome, either in the antenatal period or shortly after birth, can be a difficult time for parents. If your baby has been diagnosed with Down Syndrome, you may feel a range of emotions, including deep sadness, despair, surprise, guilt, and/or anger. You may wonder why this has happened and it is important to remember that nothing you did or did not do, caused it. Instead, focus on the incredible journey, filled with love and learning, that you are about to embark on.
Health Issues Associated with Down Syndrome
- Heart defects: As many as 50% of the babies with Down Syndrome are also born with heart defects. As with any condition, it’s severity can range from mild to severe. Babies with major heart defects may experience heart failure shortly after birth which requires immediate treatment. However, not all heart defects are immediately obvious. For this reason, your baby will have an echocardiogram (ECG) within the first few months of life to check for heart problems. Minor heart defects may be manageable with medications while major defects may require surgery.
- Thyroid function: Approx. 10% of babies born with Down Syndrome have thyroid disease. Hypothyroidism, the slowing of the thyroid gland, is the most common thyroid disease in babies with Down Syndrome. This can be treated with medication.
- Eye and Ear problems: Over 50% of babies with Down Syndrome have visual problems. In many cases, these problems can be treated with glasses or surgery. Hearing issues are common in babies with Down Syndrome. Your baby will have an audiology follow up (hearing test) and should have regular eye tests so any such problems are highlighted before they interfere with langauge development.
- Gastro-intestinal issues: Approximately 10 – 12% of babies with Down Syndrome have structural abnormalities in the gastrointestinal tract that require surgery for correction.
- Other issues: Babies with Down Syndrome have a 15-20 times greater risk of developing leukemia than babies without Down Syndrome. However, the likelihood of developing it is still relatively low. If it does occur, it generally begins within the first 3 years of life and has a high cure rate. A temporary form of leukemia is also seen in the newborn period that resolves spontaneously within the first 2-3 months of life.
Feeding Your Baby with Down Syndrome
The early days of feeding are a time for you and your baby to get to know each other. All babies are unique and parents must learn their baby’s like and dislikes when feeding. You may also need to make adjustments during feeding time to suit your baby’s physical ability. You will discover that your baby has special physical characteristics that may have an impact on their feeding. As you get to know your baby, your baby’s needs will get more obvious to you. You may not experience all, or any, of the challenges discussed here. However, understanding that babies with Down Syndrome have particular needs will help you to get feeding off to a good start.
Breastfeeding
Babies with Down Syndrome often have low muscle tone; this includes reduced muscle strength in their tongue and lips. Therefore, good head support is particularly important for your baby during breastfeeding. There are a variety of ways you can hold your baby while breastfeeding that will support their head, neck, and upper back. For example, providing gentle, steady support to the base of your baby’s head will help them to suck well, without becoming too tired. It is important that you provide gentle support because too much pressure on the back of your baby’s head will result in a poor latch onto the nipple.
Babies with Down syndrome may have a protruding tongue that can push against your nipple. This may pose a challenge for your baby when latching on because they may push the nipple out of their mouth. If your baby is latched on properly, you should be able to see their tongue cupped under the breast, resting on their lower gum. The lactation consultant in the neonatal unit is available to help you establish breastfeeding.
As with any challenge, the right information, support and encouragement will help you overcome them. If difficulties continue despite receiving support and assistance, it is ok to accept that breastfeeding may not work out for you this time.
Feeding by Bottle
Bottles are difficult to avoid if the baby is unable to maintain an effective suckle at the breast. The need for bottles may diminish as your baby matures as their muscle tone improves. Some mothers have found ways to use the bottle in a manner that supports breastfeeding. It can be a problem when a baby does not wake up enough to feed well. Some babies sleep for long periods between feeds and seem to be content even if they are hungry. Your doctor/nurse will be the best guide for you in acknowledging when, and if, your baby has had enough to eat.
Helpful Links
References
[1] Yurdakok M. (2015) Phototherapy in the newborn:Whats new? Journal of Peadiatric and neonatal individualised medicine 4(2);1-26
